 Marvin Berman, Ph.D.
Marvin Berman, Ph.D. We're pleased to welcome Marvin Berman as a guest writer. His work with depression, anxiety, addictions and learning disabilities is now augmented by his research into near-infrared light stimulation (NIRS) to the brain. As you will read, he is seeking dementia patients for a two-year study into NIRS combined with neurofeedback. In this, the International Year of Light, Dr. Berman's research is both timely and very promising for humankind.
By Marvin H. Berman, Ph.D.
A diagnosis of dementia can be terrifying to patients and their loved ones. Some psychologists are suggesting that we should not even use the word ‘dementia’ when describing test results, saying it is preferable to talk about the ‘memory challenges’ and ‘executive functioning deficits’. The wife of a patient of mine who is struggling with short-term memory loss and expressive aphasia (can’t find the right word), recently told me she feared that if her husband was told that he probably had Alzheimer’s, he might commit suicide. She therefore spent countless hours and huge sums of money trying different methods to improve his condition but wouldn’t tell him what she knew and forbade the doctors from informing him directly of his diagnosis.
But avoidance and denial create tremendous stress on the family, coloring all interactions to the point where everyone puts their energies into ensuring they don’t say something they shouldn’t. Instead of denial, families need to spend time talking about what’s really important, namely the time they spend together, including their feelings about the unknowns they are all facing as the disease progresses. Finding ways to support one another takes time and thought and support from doctors and other experts, as well as the growing dementia-support community.
What patients and families need most is a sense of hope that something can be done to stop the progression of memory loss. Several hundred drug trials worldwide have so far been unsuccessful and interest is now focusing on new alternative approaches. As a neuroscientist, clinician and researcher (I founded the Quietmind Foundation and Quietmind Associates Brain Enhancement and Treatment Center in Plymouth Meeting, PA, 15 years ago), I’ve been working with brainwave biofeedback or neurofeedback (NFB), and near-infrared light stimulation (NIRS) to the brain for the past seven years. I’m very encouraged with the results we’re seeing with these technologies and I believe they hold great promise for those affected by neurodegenerative diseases including dementia and Parkinson’s disease.
Until that time I had been working with patients using neurofeedback, which is EEG-based biofeedback, along with body-centered psychotherapy and computerized cognitive rehabilitation. We were getting good results with a variety of neuropsychiatric conditions, including depression, anxiety, addictions and learning disabilities. With NFB training, the patient watches a movie or listens to music with the volume and brightness controlled by the brain’s electrical activity. When the activity is within the normal range the brightness and volume are at the desired level, but when the brain produces abnormal activity the brightness and volume instantly drop by 50 percent. The brain is therefore ‘rewarded’ with the preferred volume and brightness and works to maintain those conditions, thereby learning to function in ways that are more efficient and appropriate.
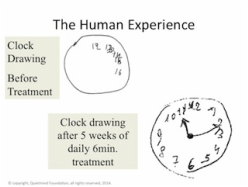
The addition of NIRS to our existing training protocol has yielded wonderful results, not only for patients with Alzheimer’s and Parkinson’s diseases but also for patients, especially veterans with traumatic head injuries and others seeking peak cognitive, athletic or artistic performance. It has been rewarding to hear patients report that they are sleeping, thinking and feeling better after a few short sessions of the combined NIRS and neurofeedback therapy. Some notice their vision and balance improving after a single six-minute training session.
The NIR stimulation is employed using a specially designed helmet containing 1200 light emitting diodes (LEDs), all designed to transmit the NIRS directly into the upper portions of the cortex and the brain stem. The daily treatments take only six minutes and involve sitting still, wearing the NIRS helmet and maintaining an upward gaze with normal blinking. No negative side effects are reported, other than some slight discomfort from the weight of the helmet which can be eliminated by hooking it to an adjustable stand. The treatment is done daily to maintain increased blood flow, oxygenation and ATP levels and thereby continues to provide additional energy to the brain.
 Amazing Progress!
Amazing Progress! Our understanding of the overall process when combining the two interventions is that the NIRS is essentially performing a repair function to the brain tissue itself, while the NFB is helping to retrain the brain’s electrical activity to function more efficiently. The repair comes from the improved health (blood flow and oxygen) of the brain tissue and increased availability of ATP. At the same time the NIRS also serves to prevent additional damage to the cells from occurring. The retraining is a result of the NFB rewarding the brain as it learns to function normally and therefore more efficiently.
Initial positive clinical results with a few patients made us anxious to conduct a double-blind, placebo-controlled clinical trial to determine the basis for the improvements we were seeing. We recruited 11 subjects to come daily for a 20-minute treatment for 28 days. We tested them before and after each session and at the start and end points of treatment. The active NIRS treatment group did better than the placebo group on several memory tests and their brainwave patterns and brain blood flow began functioning more normally. The subjects and their caregivers reported improvements in sleep, memory, organization of speech, mood stability, balance and gait.
Research at the Quietmind Foundation, along with that conducted at the neurobiological science laboratories at Durham University and at neurological clinics in South Africa have confirmed that this type of stimulation can positively influence neurodegenerative processes, both in terms of improving memory and maintaining a more stable positive mood. Active treatment subjects also showed improvement in memory for lists of words, and in retaining and following verbal instructions.
The requisite first step in gaining support for human clinical trials was our demonstration that white blood cells and nerve cells pretreated with infrared light and then exposed to toxic chemicals fared far better than the same cells pretreated with standard light. Animal studies showed that mice who quickly developed the beta amyloid plaques and showed significant memory problems improved in their performance in memory trials after treatment with the infrared light compared to mice that didn’t get NIR stimulation.
Subjects are currently being recruited for two-year, single-subject clinical trials of the combined home-based neurofeedback and NIRS therapy. All subjects will receive the active treatment during these trials. Unfortunately, due to the absence of outside funding, participants will be required to pay $7,500/year to participate. The fee covers all equipment, assessment, training and supervision costs. Subjects can live anywhere as long as they have a reliable high-speed Internet connection and caregivers are available to hook up the neurofeedback training electrodes and operate the NIRS helmet and neurofeedback software. Subjects can either come to Quietmind Foundation’s clinic for pre- and post-treatment assessments or assessments can be arranged through local psychologists and psychiatrists.
Interested parties can contact the Quietmind Foundation at: http://quietmindfdn.org, or call 610-940-0488.
